Approach to Abdominal Pain Powerpoint Abdominal Pain Causes Funny Images
See also
Adolescent gynaecology - lower abdominal pain
Acute scrotal pain or swelling
Constipation
Intussusception
NB Cases of PIMS-TS - a novel post-infectious systemic hyperinflammatory syndrome - have been reported in children in Victoria. See alert
Key points
- Repeated examination is useful to look for the persistence or evolution of signs and evaluate response to treatment
- Analgesia should be used and will not mask potentially serious causes of pain
- Investigations are guided by the most likely cause. Most children do not need investigations
- True bilious vomiting is dark green and warrants urgent surgical input
Background
- The key consideration in acute abdominal pain is the differentiation between surgical and non-surgical causes
- Non-specific abdominal pain is very common but is a diagnosis of exclusion once red flags are considered. See Additional notes section below for more details
- Symptoms in neonates may be attributed by parents as abdominal pain. A thorough examination and a broad differential should be considered in this group. See Unsettled baby
Common and time critical causes of abdominal pain by age
Important non-abdominal causes of abdominal pain to consider:
DKA
Headache (Migraine)
Henoch Schonlein Purpura
Hip pathology
Pneumonia
Psychological factors
Sepsis
Sexually transmitted infection
Sickle Cell Disease (vaso-occlusive crisis)
Toxin exposure or overdose
UTI/pyelonephritis
Assessment
History
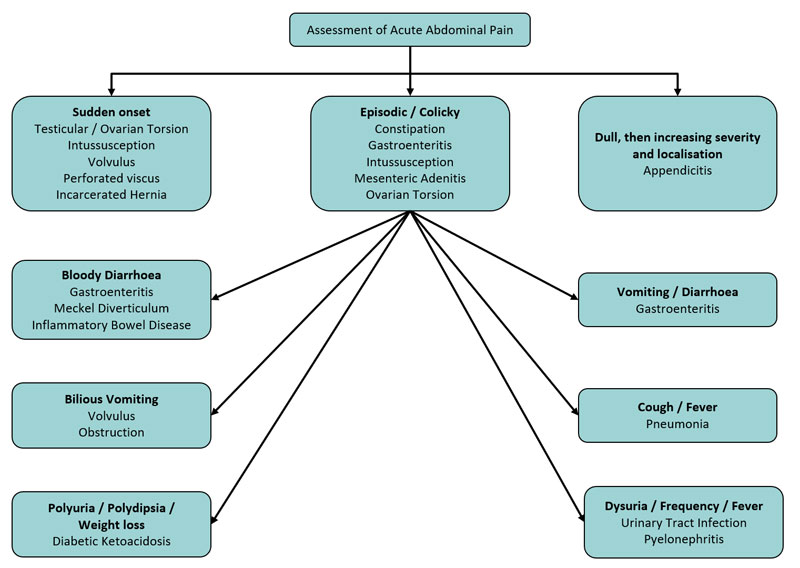
Symptoms and signs with associated differential diagnoses (the following diagram is not an exhaustive list and presentations can overlap)
Relevant past medical history
| Underlying condition | Potential complications causing abdominal pain |
| Hirschprung disease | Enterocolitis |
| Cystic fibrosis | |
| Liver disease and/or ascites | Primary bacterial peritonitis |
| Nephrotic syndrome | |
| Splenectomy | |
| VP shunt | |
| Chemotherapy | Pancreatitis |
| On immunosuppressants | |
| PEG / NG / NJ fed | |
| Inflammatory bowel disease (especially if concurrent Clostridium difficile) | Toxic megacolon |
| Immunocompromised | |
| Sickle cell disease | Vaso-occlusive crisis |
Examination
- Observe the child's movements, gait, position and level of comfort
- Examine the abdomen for:
- focal vs generalised tenderness
- rebound tenderness*
- guarding or rigidity*
- abdominal masses
- distension
- palpable faeces
- Assess for non-abdominal causes (list above)
*Peritonism:
- Child will often not want to move in the bed and will be unable to walk or hop comfortably, and will have abdominal tenderness with percussion, internal rotation of the right hip can irritate an inflamed appendix
Rectal or vaginal examination is rarely indicated in a child, this should be discussed with a senior clinician and if needed should only be performed once
Management
Investigations
Most children need no investigations
Investigations to consider, depending on differential diagnosis, may include:
- urine analysis (+/- culture +/- pregnancy test if indicated)
- electrolytes +/- LFTs
- lipase for pancreatitis
- venous blood gas
- blood sugar for DKA
- LFTs, lipase and UEC in abdominal injury
- imaging
- AXR if obstruction suspected. It isnot helpful in diagnosing constipation
- CXR if pneumonia is suspected
- Ultrasound may be requested after discussion with a senior clinician (very low yield if used indiscriminately)
- It isnot clinically indicated for testicular torsion and may delay time critical surgery
- May be appropriate in suspected ovarian torsion
- Useful if the history is suggestive of intussusception, even if examination is normal
Treatment
Treatment will be guided by the likely aetiology
- Fluid resuscitation may be required (see Intravenous fluids)
- Provide adequate analgesia. IV morphine or intranasal fentanyl may be required as initial analgesia in severe pain (see Acute pain management)
- Keep children fasting. Consider enteral or intravenous fluids if assessment or diagnosis is delayed (consult local fasting guidelines)
- Early referral of children with possible diagnoses requiring surgical or gynaecological management
- Consider a nasogastric tube if bowel obstruction is suspected
Consider consultation with local paediatric / surgical team when
- Surgical cause suspected
- Severe pain not responding to analgesia
- Child requiring admission
Consider transfer when
Child requires care beyond the comfort level of the local hospital
Note: Prior to transferring infants or children with possible surgical conditions, ensure the child has adequate analgesia, venous access and intravenous fluids
For emergency advice and paediatric or neonatal ICU transfers, see Retrieval Services .
Consider discharge when
- There are no concerning clinical features
- Presentation consistent with non-specific abdominal pain (see Additional notes below)
- A clear follow-up plan has been arranged, often with a local GP
- Parents have been given advice regarding when to seek medical attention
Parent information
Abdominal pain
NSW Children's Hospital Fact Sheets
Additional notes
Appendicitis in young children
- Often a late diagnosis
- May not present with classical symptoms
- Often presents as perforation or sepsis
- Requires careful attention to fluid and antibiotic management
Non-specific abdominal pain
- Some children suffer recurrent non-specific abdominal pain, with no organic cause identifiable
- Occurs in 10-15% of children (usually primary school aged)
- Diagnosis can only be made if pain remits completely and there is no associated vomiting, fever and change in bowel habit or oral intake
- Psychological factors (eg family, school or other stressful issues) need to be considered in some cases
- Investigations are usually not indicated
- Non-pharmacological measures (reassurance, relaxation, rubbing and heat packs) can be tried and often help
- Follow-up is important. Consider outpatient general paediatric / adolescent referral
Last updated November, 2019
Source: https://www.rch.org.au/clinicalguide/guideline_index/Abdominal_pain/
Postar um comentário for "Approach to Abdominal Pain Powerpoint Abdominal Pain Causes Funny Images"